Study finds Hepatitis C continues to raise risk of death even after cure
Thu 03 Aug 2023, 23:39:53
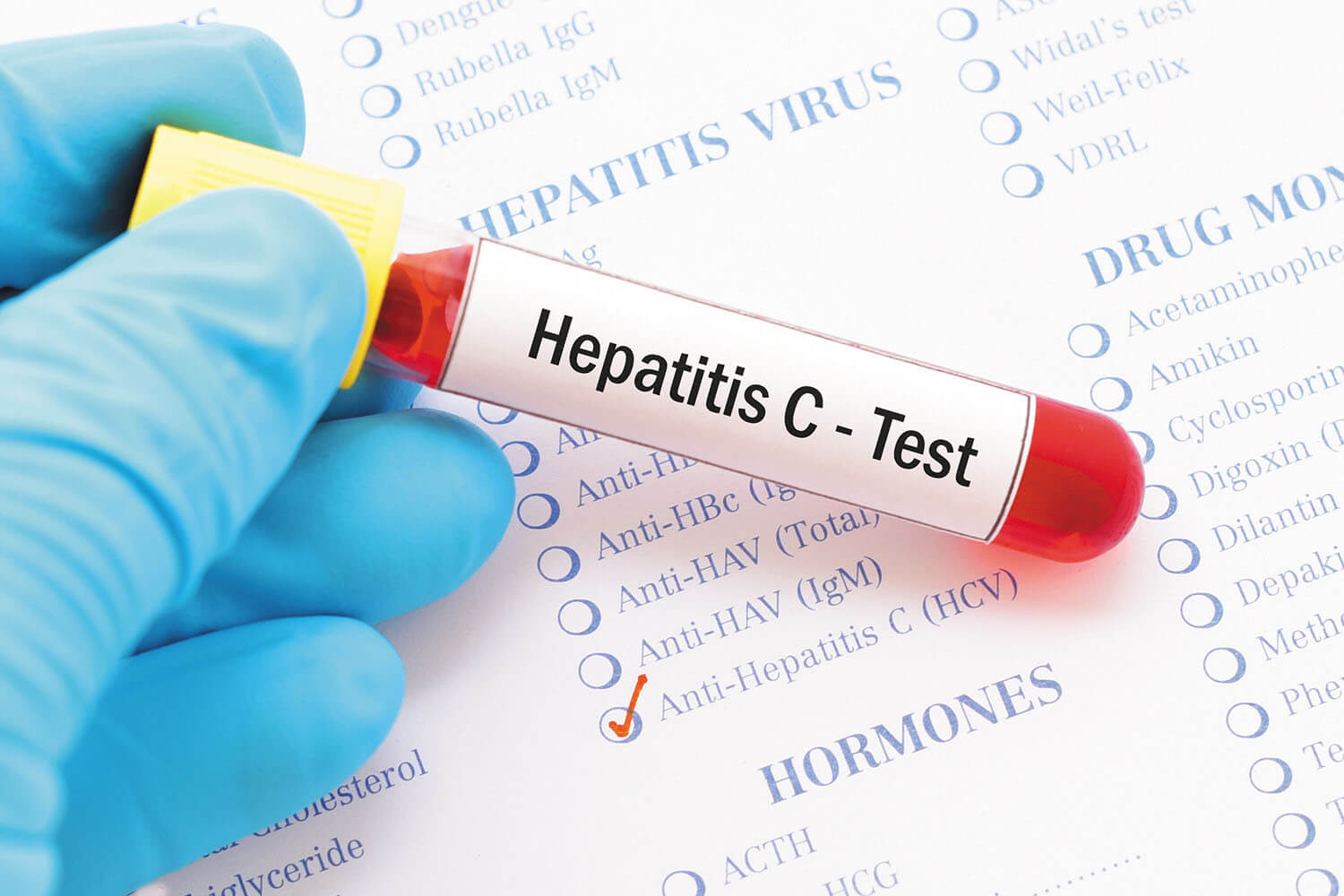
Hepatitis C is a serious viral infection that affects the liver. It is spread through contact with the blood or body fluids of an infected person, which can occur through sharing needles, having unprotected sex, or through contact with contaminated surfaces. Symptoms of hepatitis C can include jaundice, fever, fatigue, abdominal pain, nausea and sometimes joint pain. If left untreated, it can cause serious complications including liver damage, cirrhosis, and even cancer.
Treatment for hepatitis C involves antiviral medications which can reduce the viral load and clear the virus from the body. It is important to get tested for hepatitis C to determine if treatment is necessary and to prevent the spread of the virus.
Now, a recent study published by The BMJ has found that individuals, who have been cured of hepatitis C infection, still face a substantially greater risk of death compared with the general population -- between three and 14 times higher depending on liver disease stage.
The study is based on data from more than 20,000 patients with a hepatitis C cure.
The findings by Glasgow Caledonian University in Scotland and British Columbia Center for Disease Control in Canada showed that drug and liver-related causes of death were the main drivers of excess deaths and highlight the importance of continued support to fully realise the benefits of a hepatitis C cure.
Hepatitis C is a virus that can infect the liver which, if left untreated, can cause serious and potentially life-threatening liver damage over many years.
Historically, hepatitis C was treated with interferon-based therapy, which was often ineffective.
But in 2011, new medications called direct-acting antivirals (DAA) were developed. Now more than 95 per cent of patients treated with DAAs achieve a "virological cure" and have a significantly lower risk of death than untreated patients.
Yet the question of what prognosis cured patients can expect compared with the general population remains the subject of
debate.
debate.
To explore this further, a team of the UK and Canadian researchers set out to measure mortality rates in individuals with a hepatitis C cure and assess how these rates compare with the general population.
They analysed data from three population studies carried out in British Columbia (Canada), Scotland and England involving 21,790 individuals who achieved a hepatitis C cure between 2014 and 2019.
Most participants did not have cirrhosis at cure. The average age of pre-cirrhosis patients in Scotland was 44 years and 56 years in British Columbia.
A total of 1,572 (7 per cent) of participants died during follow-up. The leading causes of death were drug-related (24 per cent), liver failure (18 per cent) and liver cancer (16 per cent).
After taking account of age, death rates were considerably higher than the general population across all disease severity groups and settings.
Rates also increased appreciably with liver disease severity.
For patients without cirrhosis, the leading cause of excess death was drug-related, whereas, in patients with cirrhosis, the two leading drivers were liver cancer and liver failure.
Across all disease stages and settings, older age, recent substance use, alcohol use and pre-existing conditions (co-morbidities) were associated with higher death rates.
These are observational findings and the researchers acknowledge that they may not apply to all settings, particularly where injecting drug use is not the dominant mode of hepatitis C transmission.
However, this is the largest and most representative study performed to date and the researchers say their results "show unequivocally that cured patients continue to face substantial mortality rates, driven by liver and drug-related causes."
As such, they highlight the importance of establishing robust post-cure follow-up pathways, as well as services and interventions to prevent drug and alcohol-related harms, to fully realise the benefits of a hepatitis C cure.
No Comments For This Post, Be first to write a Comment.
Most viewed from Health
AIMIM News
Latest Urdu News
Most Viewed
May 26, 2020
Do you think Canada-India relations will improve under New PM Mark Carney?
Latest Videos View All
Like Us
Home
About Us
Advertise With Us
All Polls
Epaper Archives
Privacy Policy
Contact Us
Download Etemaad App
© 2025 Etemaad Daily News, All Rights Reserved.